Vasculogenic mimicry, a process in which tumor cells can form structures that resemble blood vessels and that can serve as blood conduits, is a common feature in malignant mesothelioma, according to a recent study published in Pathology.
The findings from the study, “Vasculogenic mimicry in malignant mesothelioma: an experimental and immunohistochemical analysis,” may lead to the development of more specific and targeted treatment approaches that combine anti-angiogenic drugs with other agents that prevent mesothelioma cells from incorporating these vessel-like structures, to destroy tumor blood supply.
Traditionally, researchers believed that the tumor vascular system was derived from pre-existing vessels that grew to form new vascular channels in response to signals from the tumor cells. Though this mechanism also contributes to tumor angiogenesis, new research emerged showing that tumor cells can re-differentiate to endothelium-like cells (endothelial cells are the cells that line blood vessels) and form hollow channels through which blood can flow.
This mechanism, called vasculogenic mimicry, was first described in uveal melanomas, but has been observed in several other tumors and associated with poor prognosis. In malignant mesothelioma, however, it is unclear whether vasculogenic mimicry is also present.
To address that, researchers cultured mesothelioma cells, obtained from pleural effusion fluids, in a matrix that is known to induce tube-formation in endothelial cells. Importantly, they found that all 12 primary mesothelioma cell lines could form tubes in that matrix. However, this capacity was not observed in normal mesothelial cells.
Consistently, when mesothelioma cells were placed on the matrix together with normal endothelial cells, these cells formed interconneted networks composed of both cell types, suggesting that mesothelioma cells could incorporate normal blood vessels.
The researchers then looked at the tumor blood vessels found in both a mouse mesothelioma model and in human samples.
Mice with human mesothelioma tumors confirmed the in vitro results. Indeed, the researchers found that the tumor blood vessels in these mice were composed of cells of both human and mouse origin.
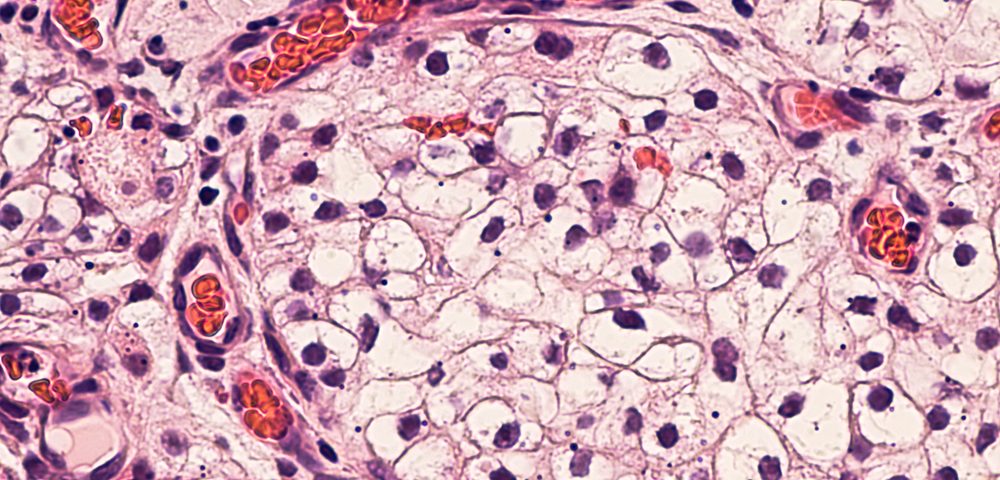
This suggested that these vessels were being formed by pre-exiting mice vessels, but that the human tumor cells were also incorporating these structures. Some vessels were even composed exclusively of human cells, suggesting the tumor cells could generate their own vasculature.
Interestingly, although the mesothelioma cells in the vessels did not lose the expression of mesothelioma markers, they started expressing a protein that is typically seen in endothelial cells.
Similar results were found in biopsy samples from four mesothelioma patients, pointing to vasculogenic mimicry as a routine occurrence in mesothelioma, with the ability of tumor cells-derived blood vessels to interconnect with host blood vessels.
“If vascular mimicry in mesothelioma can be characterized more fully, this may facilitate identification of more specific and targeted therapeutic approaches such as anti-angiogenesis in combination with chemotherapy and immunotherapy or other therapeutic approaches,” the researchers wrote.