Analyzing the levels of microRNA (miRNA)-130a in cells collected from pleural effusions, a condition in which fluid accumulates between the thin membranes surrounding the lungs, may help distinguish malignant pleural mesothelioma from lung adenocarcinoma.
The study, “miR-130A as a diagnostic marker to differentiate malignant mesothelioma from lung adenocarcinoma in pleural effusion cytology,” was published in the journal Cancer Cytopathology.
Patients with malignant pleural mesothelioma have a poor prognosis and often present recurrent pleural effusions, a condition in which excess fluid builds around the lung. The major cause for malignant pleural effusions, however, is lung adenocarcinoma.
Current methods for diagnosing these diseases may overlap, meaning there is the need for more specific and reliable markers for distinguishing malignant pleural mesothelioma from lung cancer.
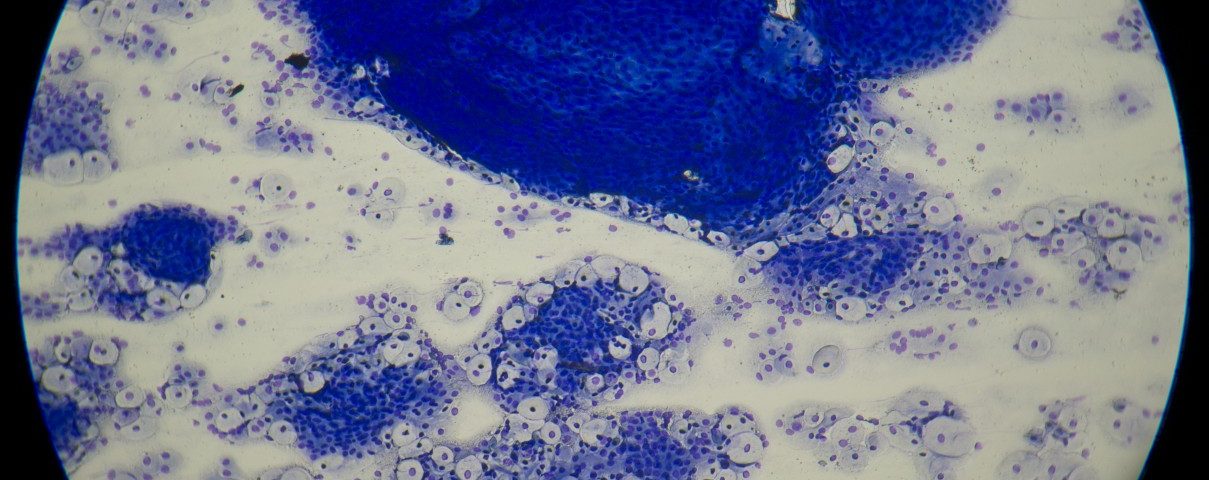
Researchers investigated if analyzing miRNAs expression could prove effective as a diagnostic tool for distinguishing both tumor types. miRNAs are a special class of short RNA molecules reported as tumor-specific. Moreover, their analysis can be performed on cytologic smears (thin tissue or blood samples spread on a glass slide) from patients, to aid the diagnosis.
First, researchers performed a bioinformatic analysis of data collected from The Cancer Genome Atlas (TCGA). In total, they analyzed 1,047 miRNAs and corresponding clinical information for lung cancer (511 cases) and malignant pleural mesothelioma (87 cases).
Two additional other data sets regarding the expression of 1,111 miRNAs were collected and included 35 malignant pleural mesothelioma and 25 lung cancer samples. The analysis identified the most differentially expressed set of miRNAs in each tumor type. The expression of the candidates was later confirmed by another technique in samples from patients with malignant pleural mesothelioma and lung cancer.
Of all the microRNAs tested, six – miR-130a, miR-193a, miR-675, miR-141, miR-205, and miR-375 – were categorized as the best distinguishing markers. But only miR-130a expression was found significantly increased in malignant pleural mesothelioma samples, relative to those of lung cancer. Specifically, researchers found that miR-130a showed a sensitivity of 77%, a specificity of 67%, a positive predictive value of 69%, a negative predictive value of 75%, and an accuracy of 72% in identifying malignant pleural mesothelioma. A positive predictive value measured the probability that subjects with a positive screening test are indeed carrying the disease.
Overall, the results support that “miR-130a quantification could be used reliably as second-level diagnostic tool to differentiate malignant pleural mesothelioma from lung adenocarcinoma,” researchers concluded. Additional studies with larger samples are, however, required to confirm these initial results, they said.