Long-term localized chemotherapy may significantly improve survival in patients with malignant peritoneal mesothelioma (MPM), according to a study.
The research, “Long-Term Regional Chemotherapy For Patients With Epithelial Malignant Peritoneal Mesothelioma Results In Improved Survival,” was published in the European Journal of Surgical Oncology.
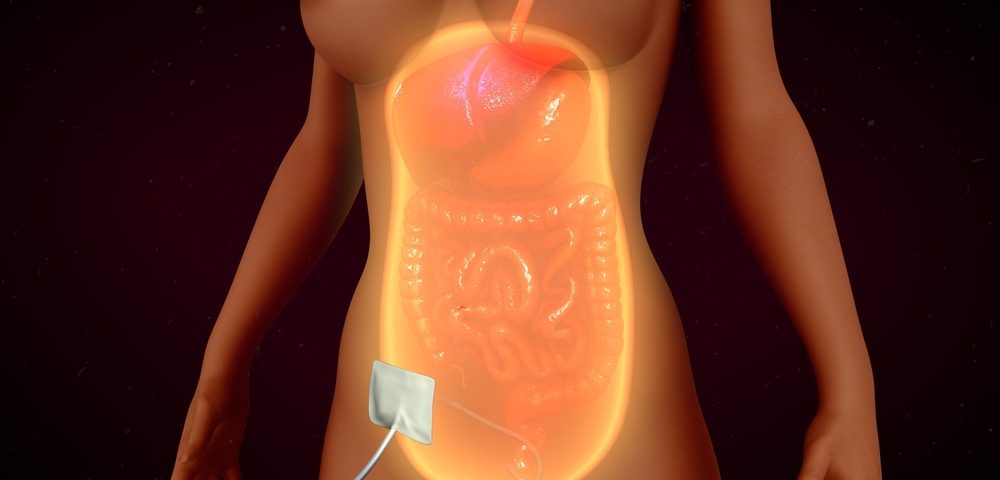
Malignant peritoneal mesothelioma affects the peritoneal cavity, a fluid-filled gap between the abdomen’s walls and organs. Patients are usually treated with cytoreductive surgery (CRS) to remove cancer from the abdomen and pelvis.
Studies have suggested that adding peritoneal chemotherapy could improve patients’ outcomes.
Three types of chemotherapy have been used to evaluate whether chemo can improve surgery’s effectiveness. At one point, patients were treated with hyperthermic perioperative chemotherapy (HIPEC) with Adriamycin (doxorubicin) and Platinol (cisplatin). The therapy was administered during surgery.
Later, patients received HIPEC together with early postoperative intraperitoneal chemotherapy (EPIC) with Taxol (paclitaxel) in the first five days after surgery.
More recently, patients have received HIPEC, then EPIC, then long-term intraperitoneal (IP) Taxol or IP Alimta (pemetrexed) plus intravenous (IV) Platinol as an adjuvant intraperitoneal chemotherapy (NIPEC). Adjuvant chemotherapy is administered after a cancerous tumor is removed.
“The overall strategy [was] to achieve a complete response through the use of surgery and then maintain that response through the use of regional chemotherapy,” the researchers wrote.
To assess which of the three approaches provided better survival outcomes, researchers analyzed the medical records of 129 MPM patients who received CRS followed by one of the chemotherapies.
Forty-two patients had received HIPEC, 58 patients EPIC and HIPEC, and 29 patients HIPEC, EPIC, and NIPEC over 20 years.
The five-year survival rate was 44% of patients with HIPEC, 52% with EPIC and HIPEC, and 75% with HIPIC, EPIC, and NIPEC. Researchers found that only those patients receiving all three types of chemotherapy showing a significantly longer survival rate than those receiving CRS plus HIPEC.
Factors such as age, gender, treatment administered, peritoneal cancer index (PCI) score, and how completely cancer cells were removed significantly influenced patients’ outcomes.
“Over a 20-year time span these 3 groups of patients underwent increasingly aggressive regional cancer chemotherapy treatments,” the researchers wrote. “Adding EPIC to HIPEC showed no significant improvement; however, a statistically significant increase in survival resulted when multiple cycles of NIPEC were initiated.”
Researchers pointed out that “survival” was not necessarily the same as “progression-free survival,” which was not assessed in their study.
They also noted that their study had limitations. One was the relatively small number of patients treated with NIPEC. Another was that the localized chemotherapy regimens that doctors used might have been different from patient to patient — a suggestion that NIPEC’s benefits may have been seen in patients from a single institution only.
Researchers called for multi-institutional studies to confirm their finding that NIPEC helped improve patients’ outcomes.