Elevated platelet levels in malignant peritoneal mesothelioma (MPM) patients being considered for surgery is associated with poor outcomes, a cohort study shows.
The study, “Preoperative Thrombocytosis Predicts Shortened Survival in Patients with Malignant Peritoneal Mesothelioma Undergoing Operative Cytoreduction and Hyperthermic Intraperitoneal Chemotherapy,” was published in the journal Annals of Surgical Oncology.
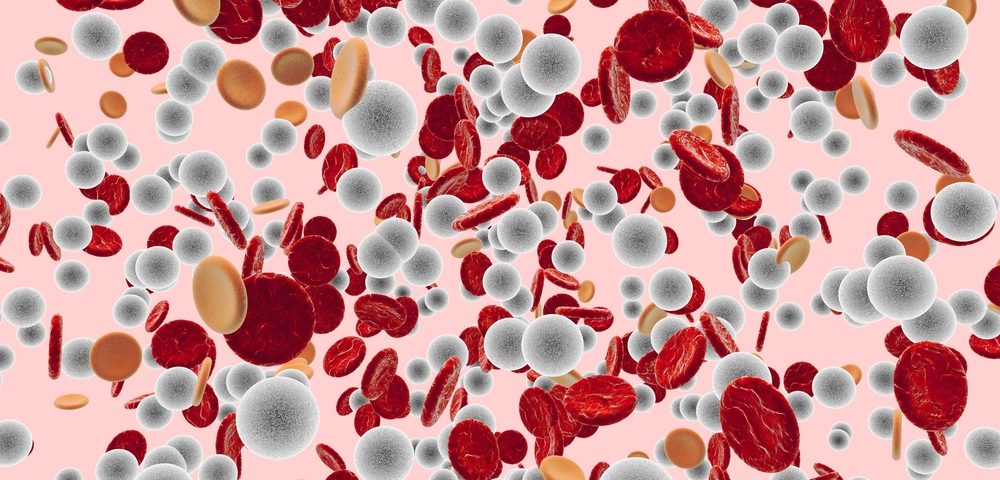
Thrombocytosis describes a condition characterized by above-normal platelet counts. Platelets are key components of blood that help form clots to stop bleeding.
In several cancers, thrombocytosis was identified as a negative prognostic factor. However, the clinical significance of a prior condition of thrombocytosis in patients with MPM remains unaddressed. Moreover, “it is unknown whether thrombocytosis directly predicts poor prognosis or is a surrogate for other prognostic factors, such as disease burden or extent of surgical resection,” researchers wrote.
Now, researchers at the Greenebaum Comprehensive Cancer Center investigated the effects of preoperative platelet counts in patients undergoing surgical resection for high-grade MPM. Additionally, they also investigated a potential association between preoperative thrombocytosis and other factors that may contribute to overall survival.
They reviewed data from 100 patients (47 women and 53 men) with high-grade epithelioid MPM who underwent surgical cytoreduction (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) between 2006 and 2015 at their institution. HIPEC is a therapeutic strategy usually performed in combination with surgery, and is characterized by the infusion of warmed anti-cancer drugs into the peritoneal cavity. Combining both CRS and HIPEC has been shown to prolong survival in certain patients with MPM.
The study showed that high levels of platelets before surgery was a predictor of shortened survival in patients with MPM undergoing CRS and HIPEC: the median overall survival in patients with higher versus normal platelet counts were 13 months and 58 months, respectively.
Also, researchers observed that in this patient population, thrombocytosis appears to reflect a more aggressive tumor.
Patients with higher platelets counts also seemed more likely to undergo an incomplete tumor resection, which may suggest more aggressive tumor.
“Although there is a strong association between incomplete cytoreduction and preoperative thrombocytosis, this alone is not sufficient to account for the differences in survival between the groups,” researchers wrote.
Overall, the results of this group study suggest that high platelet counts in patients with MPM is linked to poor outcomes. As such, “patients with MPM and baseline thrombocytosis are not good candidates for immediate CRS and HIPEC,” the study concluded.


One comment